One of the leading causes of blindness is glaucoma, a condition defined as damage to the optic nerve cells. Because glaucoma has no noticeable symptoms, early diagnosis and successful treatment of glaucoma require regular exams and glaucoma test results.
Glaucoma progresses gradually. It can cause irreversible damage to the optic nerve that could lead to vision loss or trouble doing everyday tasks, such as driving.
How often should you be tested for glaucoma? In general, if you are older than 40 and have a family history of the disease, WebMD suggests an eye exam every one or two years. If you have glaucoma in your family or a condition that could contribute to the disease, such as diabetes, you may need to be checked every year.
This article explores tests, how to tell if you have abnormal glaucoma test results, and what they mean for you.
Visual Field Test
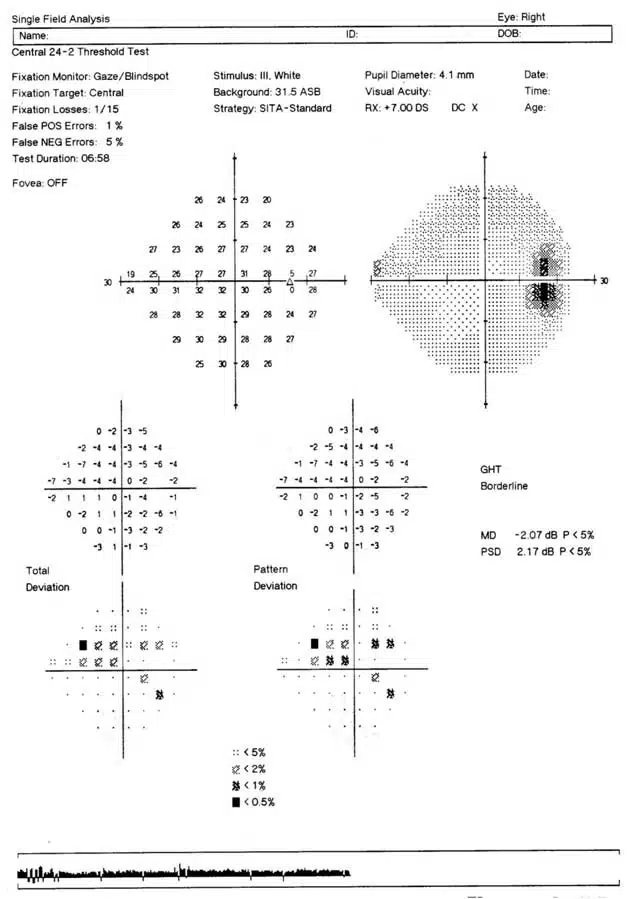 Because glaucoma can cause peripheral vision loss, a visual field test may be done to measure your peripheral vision.
Because glaucoma can cause peripheral vision loss, a visual field test may be done to measure your peripheral vision.
There are various ways to perform a field vision test, but usually, one eye is tested at a time using a specialized instrument. The test begins when you’re seated in front of a machine, looking into it, and focusing on the light ahead. During the test, a faint light will appear momentarily at different positions in your field of vision. You will be asked to press a button each time you detect the light.
If you’re having trouble identifying flashing lights of various sizes and intensities, that may be a sign that you have glaucoma. Worse results over time may indicate glaucoma progression.
Ask your eye doctor to explain the exam and test results so you know whether or not you’re experiencing peripheral eyesight loss.
Optic Nerve Photography
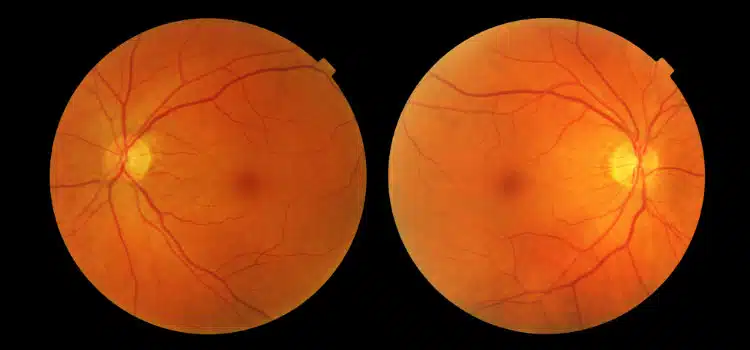
Glaucoma indicates damage to the optic nerve and nerve fiber layer. Optic nerve photographs show optic nerve damage over time. Your eye doctor will evaluate optic nerve photographs to identify abnormalities and compare the health of the optic nerve in follow-up exams. If the optic nerve has abnormalities, it’s likely a sign of glaucoma.
Optic nerve photography is crucial because elevated eye pressures are not always present in patients who have a type of open-angle glaucoma called normal tension glaucoma. Patients with this condition have IOP within a normal range but continue to lose the field of vision. Normal Tension Glaucoma is often vascular in origin, associated with other vasculopathy, and often caused by systemic hypotension while sleeping. Optic nerve photographs will be taken during the patient’s initial examination, then at least annually or more often if changes are noted.
Optical Coherence Topography Test
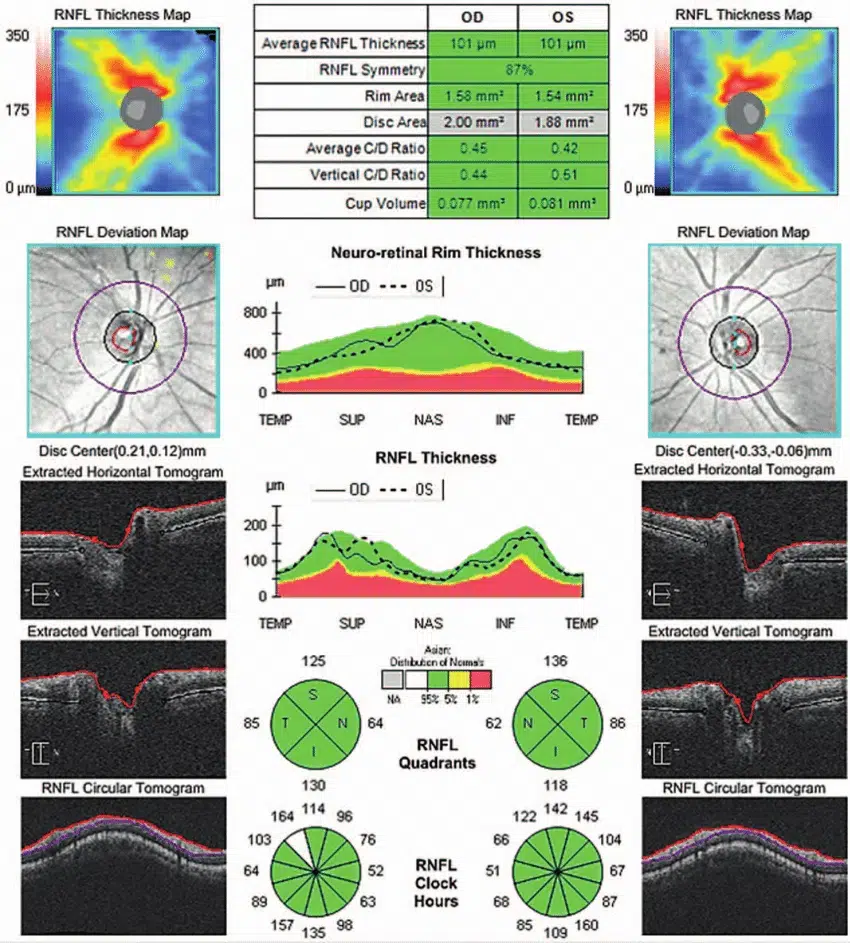
Optical coherence topography (OCT) tests obtain a topographical map of the optic nerve, using non-invasive light waves to take cross-section pictures of the retina. An OCT test measures the thickness of the nerve fiber layer, which is the portion of the optic nerve most vulnerable to eye pressure elevation.
An OCT test is taken at the patient’s initial exam and then every 6 to 12 months after. Thinning of the optic nerve indicates that it is being damaged by elevated intraocular pressure. When OCT test results show that the optic nerve is thinning, this is a symptom of glaucoma.
In addition to glaucoma, OCT is useful in diagnosing other eye conditions such as diabetic retinopathy and age-related macular degeneration.
Tonometry
Tonometry is a test used to measure pressure inside the eyes. The test requires eye drops that anesthetize the eye, while a small device touches the eyeball to test the eye pressure.
According to the Glaucoma Research Foundation, the range for normal pressure is 12 – 22 mm Hg. When the pressure exceeds 22 mm Hg, that usually indicates an abnormal glaucoma test. People with pressure around 16 mm Hg or higher may also be at risk for normal tension glaucoma.
Because glaucoma is a complex condition, intraocular pressure (IOP) measurements from tonometry are only one set of glaucoma test results that an eye doctor will consider when deciding on a final diagnosis.
Ophthalmoscopy

Eye Doctor conducting an ophthalmoscopy test
During an ophthalmoscopy test, eye drops are used to dilate the pupil. Your doctor will look into your eye with a device that has a light to magnify the optic nerve.
If the optic nerve’s shape and/or color doesn’t look normal, or the pressure within the eye is higher than the normal range, your doctor may perform more exams to double-check the abnormal glaucoma test results and be certain of the diagnosis.
Gonioscopy
Proper eye pressure is maintained by the constant production and drainage of eye fluid. When the drainage system isn’t working, eye pressure can increase and damage the optic nerve, resulting in glaucoma.
A gonioscopy test evaluates the eye’s internal drainage system. To do this, a special lens enables the eye doctor to see the drainage system.

Four mirror mini gonio lens (Source: Ocular Instruments)
Abnormal glaucoma test results from a gonioscopy test may include:
- Irregularities in the drainage system, particularly a closed angle, which can lead to sudden or rapid increases in eye pressure
- Abnormal blood vessels
- Adhesions
- Eye drainage system damage
This type of glaucoma test is painless and takes just a few minutes. An eye doctor uses a slit lamp, which is a special microscope used to view the eyes.
Pachymetry

Sourced from Reichert
Because thin corneal thickness can increase glaucoma risk, pachymetry is a glaucoma test used to measure corneal thickness.
During a pachymetry test, a probe called a pachymeter is placed on the front of the eye and the corneal thickness is measured. If it’s thinner than average, that means additional glaucoma tests may be beneficial. If it thins over time, that may indicate abnormal glaucoma test results.
Next Steps After You Have Your Results
If your glaucoma test results indicate elevated IOP, you are likely a glaucoma suspect. But, to arrive at a diagnosis of glaucoma, you must consult an eye doctor. Even with a high IOP, if you have a thick cornea, the measurement could be artificially high.
The best option to manage glaucoma and overall eye health is to have an annual medical eye exam and work with an eye doctor who can map out the changes in your vision over time. When your doctor makes a diagnosis, the results of each test will be taken into consideration to determine whether or not you have the disease, the stage of your condition, and if the illness is progressing.
If you have questions about abnormal glaucoma test results, what your test results mean, or what tests you can expect if you’re still in the discovery phase of your eye care journey, call or contacts us today with an eye doctor today.
Sources:
Harold A. Stein MD MSC (Ophth) FRCS(C) DOMS (London), Raymond M. Stein MD FRCS(C), Melvin I. Freeman MD FACS, 2018, Elsevier, The Ophthalmic Assistant: A Text for Allied and Associated Ophthalmic Personnel 10th Edition, Pg. 403.
